849
Views & Citations10
Likes & Shares
Background: Lung is an essential organ as it works all the time even during sleeping. Observing any abnormality inside the lung can be really truly deteriorating and may eventually lead to death. Besides, due to the recent globalization and standardization, cancers are evaluating all over the world and currently it seems like epidemic diseases. Lung or pulmonary cancers are the prime causes of death worldwide.
Method: Our aim was to investigate the role of CT-scan to identify possible pulmonary cancers. We have investigated more than eighty patients who visited radiology departments and took either chemotherapy or surgery. Our study has been correlated with detection methods of pulmonary cancers in our own set-up to ease-up therapeutic approach.
Findings: We have noticed that radiology investigations are the most effective diagnosis especially for lung cancer subjects. Our observations have also found that early stage lung carcinoma can be prevented and cured if a subject is gone through radiological investigations.
Conclusion: This study can play a major role in detecting pulmonary cancer using radiology methods and may eventually be proven as effective to prevent early stage lung cancers. Therefore, our investigations and findings may participate as an approach where oncologists and radiologists can take a decision toward suggesting an anti-cancer approach.
INTRODUCTION
Globalization and urbanization have been massively increased since the last three decades. To support the global economy, a large number of production houses and factories were built which are run through natural oils and petroleum that release many harmful gases in the environment. Besides, demand of tobacco and smoking is unimaginable especially in the urban areas [1]. Moreover, using several herbicides, pesticides and germicides for cultivation may return in human and deposit inside a vital organ that eventually end-up with various cancers. Taken together, air pollution and environmental pollutants are responsible for initiating carcinoma in the body. Among the all cancers, pulmonary cancers play the leading role causing death globally [2,3].
Clinical staging is based on the size of the lymph node as determined by CT-scan was the only noninvasive option. Even small, peripheral, small lesions, often considered to be connected with a low risk of mediastinal metastasis, frequently involve these nodes [8]. Radiotherapy is typically delivered by a peripheral beam from a linear accelerator. Standard therapy for unresectable patho-physiology consists of large time, with the dose separated over many sessions over a period of six-seven weeks, though elevated doses have been used. In normal organs, the toxic effects of radiation and radiological exposure include esophagitis, myelopathies, pneumonitis, skin desquamation, and cardiac abnormalities [9]. These harmful effects may be reduced by using three-dimensional or advanced computed tomography (CT) to guide therapy or by modulating the intensity of radiation therapy in order to spare normal tissue. Simultaneously chemotherapy may induce the effectiveness of radiation by sensitizing the tumor to radiation, but it can also increase the adverse effects too [10]. However, poor country like Bangladesh may be beneficial from the advancement of CT-scan especially for detecting pulmonary cancers in their native set-up. In CT-scan observing for lung tumor, the detected nodule frequently is either only part-solid or nonsolid, but such a nodule is to be expected to be malignant than a solid one, even when nodule size is taken into account. Therefore, this study may participate successfully in the detection and diagnosis of pulmonary cancers and their stages in countries like Bangladesh for effective treatment purposes.
METHOD
Our aim was to correlate the effectiveness role of Radiological investigations especially CT-scan in identifying pulmonary cancers. In this current study, we have followed and investigated eighty patients who visited at the respective Radiology departments in either Apollo Hospitals Dhaka or Khwaja Yunus Ali Medical College Hospital, Bangladesh. We collected their diagnosis reports and followed-up until the treatment is over or they stopped visiting for further therapy. Among the eighty lung cancer subjects, fifty-two were male and twenty-eight were female and most of them were older subjects. These numbers are too small for further scrutiny; however, we have collected all the radiological figure legends whenever they were advised to visit Radiology and Molecular Imaging Department for critical investigations. In this study only, freshly diagnosed subjects were chosen to be followed-up. We also excluded the subjects who were diagnosed with pulmonary cancers and with another organ metastasis; however, we did find several subjects who later developed metastasis. All the subjects and their radiological investigations were reported for about nine to twelve months. Along with the biochemical investigations, all eighty subjects were gone through CT-scan to detect possible carcinoma or metastasis in the pulmonary segments. By this time, we have closely gone through their investigations in the Radiology and Imaging departments such as CT-scan results. Our major objective focused only for the radiologists and oncologists while using CT-scan to detect proper carcinoma and size of the tumors. We did not try to correlate between radiological investigations and the outcomes of the therapy. In this study, more emphasis was given on the subjects who went through CT-scan for detecting possible small and non-small cell lung cancer. Among those thousand CT-scan figure legends, we have only chosen the figures which would be beneficial for our study and also for the respective health care professionals. After collecting all the representative figure legends, we used ImageJ for analyzing and finalizing the pictures to be utilized in this study.
RESULTS
DISCUSSION
Pulmonary cancer is the foremost reason of cancer death among both men and women in the USA. It is also the leading cause of cancer death among men and the second leading cause of cancer death among women worldwide. Lung cancer rates and trends vary substantially by age, sex, race/ethnicity, geography, family history and socioeconomic status because of differences in historical smoking patterns. Lung cancer mortality rates in the USA are highest among males, blacks, people of lower socioeconomic status and in the mid-South regions [11]. However, effective approaches may be a good step to reduce the treatment cost as well as case of pulmonary cancers. On the other hand, early stage diagnosis might play the prime role to cure lung tumor. CT-scan plays a major role to identify the exact size and location of lung tumors which help the overall strategy [12].
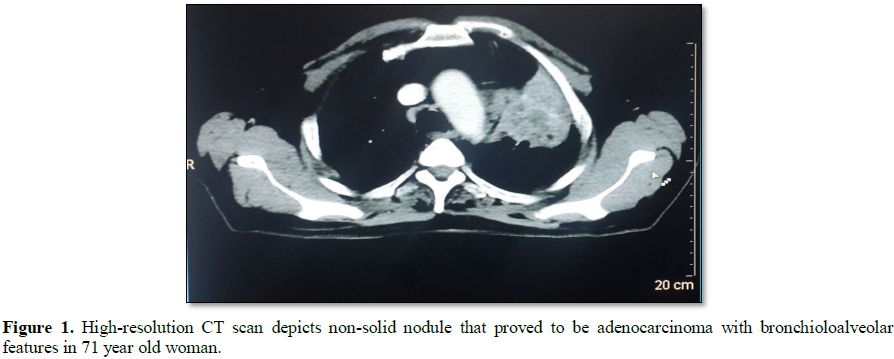
CT scan can show a tumor’s perfect shape, size, and location especially in the lung areas. It can even show the blood vessels that feed the tumor all without having to cut into the patient. By comparing CT scans done over time, oncologists and radiologists can see how a lung tumor is responding to treatment or find out if the cancer has come back after a therapy or completing the treatment. A more notable outcome in our present study, however, has to do with the impact of these nodules: overall, the frequency of malignancy in them was much privileged than in solid nodules, in the part-solid nodules in particular. In addition, the distribution by malignancy type was strikingly different in the sub-solid nodules while comparing to the solid ones. The malignancies in sub-solid nodules were typically bronchioloalveolar carcinomas or adenocarcinomas with bronchioloalveolar features, whereas in solid ones the malignancies were characteristically other subtypes of adenocarcinoma (Figure 1) [14]. Although there may be suspicion that bronchioloalveolar carcinoma represents over diagnosis of pulmonary cancer that is, that it progresses so slowly as to be inconsequential. Results of more recent studies have also suggested this development on the basis of cytologic and histologic data and studies of monoclonality and molecular markers [15]. Similarly, our study may have same anomalies to represent the figure legends.
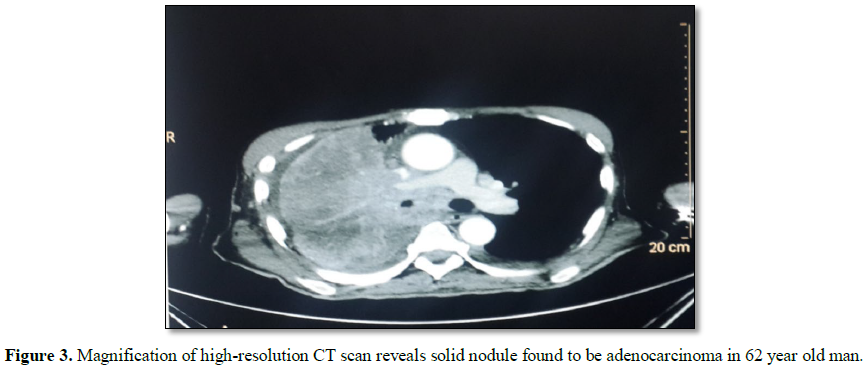
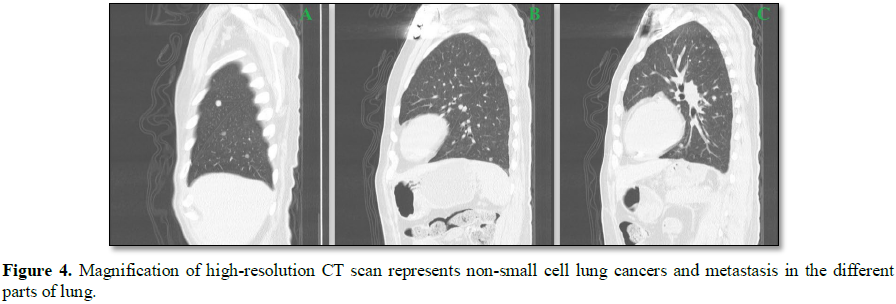
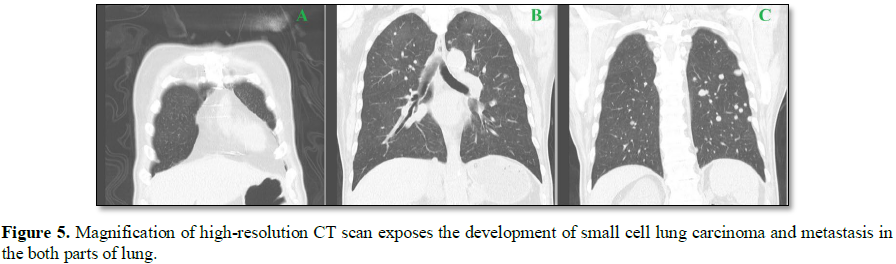
The results of this study suggested that using CT-scan can be quite effective to identify both cancer stage and location of the tumor. The figure legends may help the oncologists to suggest a therapy for a pulmonary cancer subject. Similarly, early stage of benign tumor in the alveoli can be prevented if a subject goes through regular check-up using CT-scan (Figure 2). On the other hand, both the small cell carcinoma and non-small cell carcinoma are the prime reason for death. These phases in cancer are difficult to identify because these do not provide any severe indication to be detected. The dramatic responses of patients whose disease has been refractory to all other diagnosis suggest that CT-scan may be more effective if used earlier in the course of identification. Prospective validation of CT-scan as a predictors of the responsiveness to have proper diagnosis is warranted, and immunostaining or marker analysis in the initial treatment of advanced both small and non-small cell lung cancer should now be considered (Figures 4 and 5) [16].
Therefore, because sub-solid nodules tumor, both the small and non-small cell lung carcinoma are the topic of greater significance than formerly presumed in the perspective of CT screening for pulmonary cancer, these areas need to be studied in greater detail. On the basis of our experience and that of others we think that the solid part is caused by lack of aeration in the alveoli, perhaps because the alveoli are being stressed. For further research, pooling of data is necessary to effectively verify the natural account of malignancies diagnosed in these nodules.
CONTRAINDICATIONS
Till now, there have been many cases where Radiological adverse effects reported and to some extent it is suggested that Radiology can be contra indicatory for some sophisticated subjects. Very older patients and children are not allowed for CT-scan. In this case sophisticated cancer markers or histology are suggested. It is also noticed that nausea, vomiting, constipation, irritation, elevated hypertension and appetite were also notice in the patient who had gone through CT-scan [17,18]. Besides, CT colonographic depiction identified 90% of subjects with adenomas or cancers measuring 10 mm or more in diameter, therefore, an augment published data on the role of CT colonography in reporting patients with an average risk of colorectal cancer which can be prevented at the earlier stage if possible diagnosis measure is taken as a regular health care check-up [19].
CONCLUSION
In the recent time, the incidents and mortality of cancer especially pulmonary cancers are on the verge and noticed to the primary cause for global death while considering tumor biology. This study shows a positive correlation to minimize the morbidity rate through effective diagnosis. The approach between the cancer patho-physiology and therapeutic prognosis for diagnosis might be noticeable. Our findings suggest that effective diagnosis for lung cancer subjects can be prevented if investigated in the earlier phase. Conversely, the detection technique by using Radiology may bring more fortune in near future to prevent pulmonary cancer and related tumor.
AUTHORS OBSERVATIONS
Our observations reported that lung cancers are more prominent in male subjects may be due to smoking, tobacco chewing and staying outside without protection such as masks. We have also noticed that patients, who visited in the Radiology department at earlier phase of lung tumor, were cure mostly while detecting the cancer by CT-scan. We have also reported that few subjects were diagnosed with metastasis. Many of the subjects were found to be cured after going through Radiological investigations and receiving respective therapies. Some of them were found to be very critical and later reported as dead who were diagnosed at the last stage of lung cancers. It has been also noticed that the Hospital visiting of those eighty patients were dramatic declined throughout the year, we presume that the subjects either changed the hospitals or did not want to take therapy due to tremendous expense or painful events and stress after a therapy is received or may eventually got died.
FUNDING
Our study did not receive any direct or indirect fund or grant from any governmental organizations or non-governmental agencies.
CONFLICT OF INTEREST
1. Chowdhury W, Arbee S, Debnath S, Bin Zahur S, Akter S, et al. (2017) Potent role of antioxidant molecules in prevention and management of skin cancer. J Clin Exp Dermatol Res 8: 2-7.
2. Chowdhury W, Tisha A, Akter S, Zahur S, Hasan N, et al. (2017) The role of arsenic on skin diseases, hair fall and inflammation: An immunological review and case studies. J Clin Exp Dermatol Res 8: 2-9.
3. Chowdhury NU, Farooq T, Abdullah S, Mahadi AS, Hasan MM, et al. (2016) Matrix metalloproteinases (MMP), a major responsible downstream signaling molecule for cellular damage - A review. Mol Enzymol Drug Targets 2: 2-3.
4. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet‐Tieulent J et al. (2015) Global cancer statistics, 2012. CA Cancer J Clin 65: 87-108.
5. Gazdar AF, Zhou C (2018) Lung cancer in never-smokers: A different disease. In: IASLC Thoracic Oncology edn. Elsevier 23-29: e23.
6. Dahlberg CI, Sarhan D, Chrobok M, Duru AD, Alici E (2015) Natural killer cell-based therapies targeting cancer: Possible strategies to gain and sustain anti-tumor activity. Front Immunol 30: 6-605.
7. Zou L, Wang H, He B, Zeng L, Tan T (2016) Current approaches of photothermal therapy in treating cancer metastasis with nanotherapeutics. Theranostics 6: 762-772.
8. Veiga C, Janssens G, Teng CL, Baudier T, Hotoiu L, et al. (2016) First clinical investigation of cone beam computed tomography and deformable registration for adaptive proton therapy for lung cancer. Int J Radiat Oncol Biol Phys 95: 549-559.
9. Barton K, Nickerson JP, Higgins T, Williams RK (2018) Pediatric anesthesia and neurotoxicity: What the radiologist needs to know. Pediatr Radiol 48: 31-36.
10. Beckett KR, Moriarity AK, Langer JM (2015) Safe use of contrast media: What the radiologist needs to know? Radiographics 35: 1738-1750.
11. Torre LA, Siegel RL, Jemal A (2016) Lung cancer statistics. In: Lung cancer and personalized medicine. edn. Springer, pp: 1-19.
12. Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, et al. (2002) CT screening for lung cancer: Frequency and significance of part-solid and non-solid nodules.178: 1053-1057.
13. Kitamura H, Kameda Y, Nakamura N, Nakatani Y, Inayama Y, et al. (1995) Proliferative potential and p53 overexpression in precursor and early stage lesions of bronchioloalveolar lung carcinoma. Am J Pathol 146: 876-887.
14. Noguchi M, Morikawa A, Kawasaki M, Matsuno Y, Yamada T, et al. (1995) Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer 75: 2844-2852.
15. Horeweg N, Scholten ET, de Jong PA, van der Aalst CM, Weenink C, et al. (2014) Detection of lung cancer through low-dose CT screening (NELSON): A pre-specified analysis of screening test performance and interval cancers. Lancet Oncol 15: 1342-1350.
16. Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, et al. (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350: 2129-2139.
17. Montie JE, Wood JR DP, Pontes JE, Boyett JM, Levin HS (1989) Adenocarcinoma of the prostate in cystoprostatectomy specimens removed for bladder cancer. Cancer 63: 381-385.
18. Cooner WH, Mosley B, Rutherford CL Jr, Beard JH, Pond HS, et al. (1990) Prostate cancer detection in a clinical urological practice by ultrasonography, digital rectal examination and prostate specific antigen. J Urol 143: 1146-1152.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)